“Make the best choice possible concerning what to eat in every situation.”
At the CrossFit Specialty Course: Kids, this simple statement summarizes the recommended nutritional approach for youths from 3 to 18.
Practical applications are discussed along with expectations set to reflect the broad age range and a child’s relative inability to affect family decisions.
The first, best decision is to choose real foods over processed foods, as outlined in CrossFit’s basic nutritional prescription (1): meat and vegetables, nuts and seeds, some fruit, little starch, and no sugar. This prescription helps balance intake from all macronutrient classes, ensures adequate micronutrient content, limits overall carbohydrate consumption and eliminates added sugar from the diet.
Importantly, several international groups and governments also recommend limiting added sugar. The World Health Organization (WHO) states that less than 10 percent of total daily calories should come from added sugar (2). The United States Department of Agriculture promotes a similar target (3), while the United Kingdom recommends that less than 11 percent of daily calories should come from added sugar (4).
The Australian government recommends “limiting” added sugars. The Australian government only recommends a limitation of added dietary sugar because of the lack of large, long-term studies with children; however, it acknowledges that consumption of sugar-sweetened beverages is associated with increased adiposity in children, and the drinks also might increase the risk of developing Type 2 diabetes, metabolic syndrome and dental cavities (5).
For reference, 200 calories (10 percent of a 2,000-calorie daily intake) are found in approximately 50 g or 10 teaspoons of sugar, and a 12-oz. can of Coca-Cola contains about 39 g of sugar.
The American Academy of Pediatrics notes that “as much as 40% of the daily energy consumed by 2- to 18-year-olds is in the form of ‘empty calories’ (energy-dense, nutrient-poor)(6).” This consumption data is combined with the determination that “current evidence supports the associations of added sugars with increased energy intake, increased adiposity, increased central adiposity, and increased dyslipidemia, all of which are demonstrated (cardiovascular disease) risk factors.” With that in mind, it’s no surprise the American Heart Association states that children under 2 should avoid added sugars and older children should consume less than 25 g per day (100 calories or about 6 teaspoons)(7).
 To improve health, limit consumption of added sugar. (iStockphoto.com/LemonTreeimages)
To improve health, limit consumption of added sugar. (iStockphoto.com/LemonTreeimages)
Below are some highlights of published papers showing the health benefits of adjusting overall carbohydrate quantities or even specific types of carbohydrate (including added sugar). Although these studies were conducted for short periods and with obese subjects, their results are difficult to ignore.
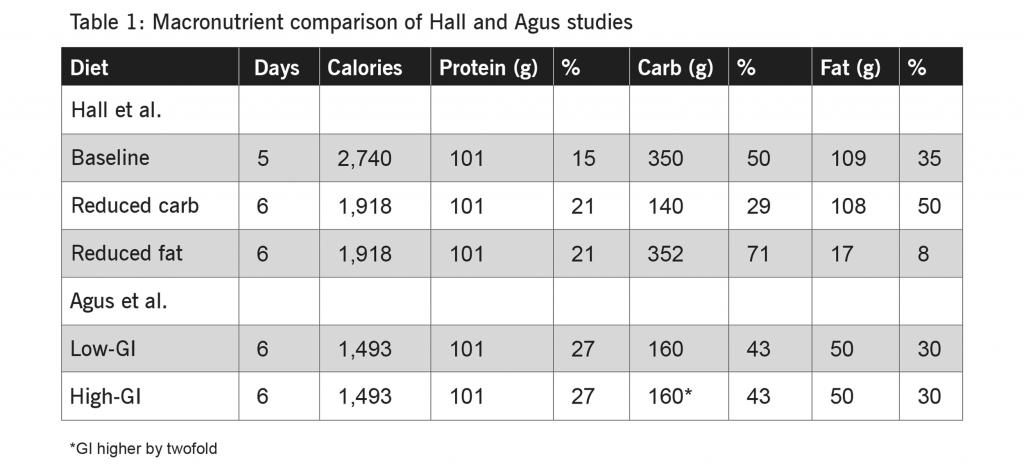
For example, Hall et al. (8) investigated the benefits of reducing total carbohydrate consumption. Nineteen obese (average BMI 35) male and female adult subjects were placed on a baseline diet (see Table 1 below) for five days. Immediately following, the group shifted to a reduced-carbohydrate diet for six days. No details were provided in the article concerning the specific components of meals, although a reduction from 350 g to 140 g of daily carbohydrate would presumably include reduced consumption of added sugar.
Twenty-two biomarkers were assessed to compare the last three days of the baseline diet to the last three days of the reduced-carbohydrate diet; 11 results were statistically significant. While only an average of 1.85 kg of weight was lost per subject, eight biomarkers were found to have improved, including insulin (22 percent reduction) and insulin resistance (40 percent reduction)(8). HDL, or “good cholesterol,” was one of the biomarkers that worsened (6 percent reduction)(8).
With a two-to-four-week separation, the study also tested the same subjects on a reduced-fat diet. For this arm of the study, the subjects lost an average of 1.3 kg per person; comparison of the 22 biomarker results showed that 10 were statistically significant. Of the 10, eight improved, such as insulin (16 percent reduction) and insulin resistance (20 percent reduction)(8). HDL (16 percent reduction) also worsened under this protocol (8).
Direct comparisons between the two protocols are confounded by the extent of the reductions; specifically, for the reduced-fat diet, fat was lowered by 84 percent compared to the baseline diet, while carbohydrate was reduced by 60 percent in the low-carb protocol.
Dietary studies can be long and very expensive to conduct. Much shorter protocols that measure biomarkers (chosen as pseudo endpoints for health changes) help to accumulate data sooner and can be used to better inform the design of larger, long-term studies. Importantly, the results from Hall et al. (8) suggest that health effects can occur somewhat independent of weight loss, at least at the onset of a change in diet. What is clear is that participants on both protocols experienced generally positive results for such a short study.
A separate article by Agus et al. (9) investigated the effects of a diet that adjusted the category of carbohydrate-containing foods consumed by subjects. Ten obese male adults (average BMI 30.6) spent six days following a low- or high-glycemic-index (GI) diet (see Table 2 above), with the latter “predicted to have a GI approximately double that of the low-GI diet” (9).
After each diet, similar amounts of weight were lost (3.62 and 3.23 kg per person). However, during the low-glycemic protocol both the glycemic and insulinemic responses were reduced by approximately 50 percent over the six days compared to the high-glycemic protocol (9), confirming the intent of lowering the GI: reducing the peaks of glucose and insulin levels.
Additionally, starting on Day 2, serum leptin remained higher in the high-glycemic diet, indicating an increase in fat stores (10). Despite this rise in leptin (generally considered an appetite suppressor) over the two days following each of the experimental diets, voluntary food intake was greater after the high-glycemic-index protocol (9). Perhaps the increased eating behavior despite increased serum leptin is due to either leptin resistance or the antagonistic action of insulin suggested by Lustig (11).
 Simple diet tip: If you keep your cart to the perimeter of the supermarket and select only fresh foods, you’re on the right track. (iStockphoto.com/Serg_Velusceac)
Simple diet tip: If you keep your cart to the perimeter of the supermarket and select only fresh foods, you’re on the right track. (iStockphoto.com/Serg_Velusceac)
Lustig et al. (12) also conducted a study with 43 children (average age 13.3 +/- 2.7 years) using an isocaloric diet where only the forms of sugar were altered compared to their self-reported diet. Specifically, total carbohydrate was kept constant but dietary sugar intake was reduced from 28 to 10 percent and fructose from 12 to 4 percent of daily calories (12).
The experimental diet was far from CrossFit’s ideal: Added sugar and fructose were replaced with “various no- or low-sugar added processed foods including turkey hot dogs, pizza, bean burritos, baked potato chips, and popcorn that were purchased at local supermarkets” (12). The intervention lasted for nine days, and various biological parameters were compared between Day 0 and Day 10. Similar to the previous studies, the participants in this study were overweight; the average BMI was 2.4 standard deviations above the average value for their age (12).
Researchers compared the results from 22 biomarker assessments from the start and end of the nine-day experiment: 14 improved and 3 worsened (the differences between the others did not reach statistical significance)(12). For example, reductions were observed for fasting insulin (31 percent reduction), insulin resistance (58 percent reduction) and fasting triglycerides (46 percent reduction)(12). On the other hand, fasting HDL cholesterol went down by 17 percent (12). The goal of the isocaloric design was to eliminate weight loss from the analysis; however, 33 of the children did lose weight (the average weight loss was 0.9 kg)(12).
In a separate analysis, Lustig et al. (12) assessed 18 biomarkers in only the 10 children who gained weight at the end of the protocol. Comparing values from the beginning and end of the experiment, six reached statistical significance, and all six improved, including fasting insulin (54 percent reduction) and insulin resistance (58 percent reduction)(12).
“In these short-term studies … , limiting total carbohydrate, skewing intake in favor of low-glycemic-index carbohydrates and restricting added sugars all showed measurable health benefits.”
In these short-term studies with overweight and obese individuals, limiting total carbohydrate, skewing intake in favor of low-glycemic-index carbohydrates and restricting added sugars all showed measurable health benefits.
The intricacies and nuances of these diets make them difficult to translate to children; the simple suggestion to eat real foods is actionable and far more understandable. Choosing real foods for the majority of meals will—at the very least—reduce the consumption of added sugars, a course of action suggested by the WHO, the American Heart Association and many others.
Within a CrossFit Kids program for youths of any age, skill work that incorporates nutrition information such as real-food identification and macronutrient classification is necessary to establish a foundation prior to any expectations of change. Best choices can only be made consistently once the various options are understood.
Additional reading: “Doctor: Your Child Doesn’t Need Sugar”
References
- Glassman G and staff. CrossFit Level 1 Training Guide. Page 17. Available here.
- World Health Organization. Guideline: Sugars intake for adults and children. Geneva: 2015. Available here.
- U.S. Department of Health and Human Services and U.S. Department of Agriculture. 2015–2020 Dietary Guidelines for Americans. 8th edition. December 2015. Available here.
- Food Standards Agency. FSA nutrient and food based guidelines for UK institutions. Revised October 2007. Available here.
- National Health and Medical Research Council. National Health and Medical Research Council (2013) Australian Dietary Guidelines. Canberra. Available here.
- Council on School Health: Committee on Nutrition. Snacks, sweetened beverages, added sugars, and schools. Pediatrics 135(3): 575-83, 2015. Available here.
- Vos MB, Kaar JL, Welsh JA, Van Horn LV, Feig DI, Anderson CA, Patel MJ, Cruz Munos J, Krebs NF, Xanthakos SA, Johnson RK. Added sugars and cardiovascular disease risk in children: A scientific statement from the American Heart Association. Circulation: 2016. Available here.
- Hall KD, Bemis T, Brychta R, Chen KY, Courville A, Crayner EJ, Goodwin S, Guo J, Howard L, Knuth ND, Miller BV, Prado CM, Siervo M, Skarulis MC, Walter M, Walter PJ, Yannai L. Calorie for calorie, dietary fat restriction results in more body fat loss than carbohydrate restriction in people with obesity. Cell Metabolism 22(3): 427-36, 2015. Available here.
- Agus MS, Swain JF, Larson CL, Eckert EA, Ludwig DS. Dietary composition and physiologic adaptations to energy restriction. American Journal of Clinical Nutrition 71(4): 901-7, 2000. Available here.
- Quest Diagnostics Test Center website. Leptin. Available here.
- Lustig RH. The ‘skinny’ on childhood obesity: How our Western environment starves kids’ brains. Pediatrics Annals 35(12): 898-902, 905-7, 2006. Available here.
- Lustig RH, Mulligan K, Noworolski SM, Tai VW, Wen MJ, Erkin-Cakmak A, Gugliucci A, Schwarz JM. Isocaloric fructose restriction and metabolic improvement in children with obesity and metabolic syndrome. Obesity 24(2): 453-60, 2016. Availble here.
All links accessed July 12, 2017.
About the Author: Jon Gary received his doctorate in molecular biology from UCLA. He is a Certified CrossFit Level 3 (CF-L3) Trainer and Flowmaster for the CrossFit Specialty Course: Kids. He has been doing CrossFit since 2003. He lives in San Diego, California, with his wife and coaches teenagers at CrossFit Escudo.
Cover image: iStockphoto.com/OcusFocus